Trigeminal Neuralgia: Comparison of Treatment Methods
Trigeminal Neuralgia: Comparison of Treatment Methods (click here)
Prospective comparison of long-term pain relief rates after first-time microvascular decompression and stereotactic radiosurgery for trigeminal neuralgia.
Abstract
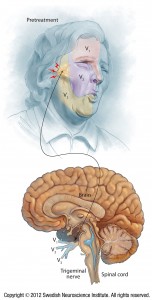
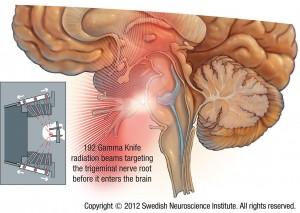
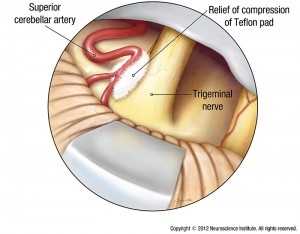
OBJECTIVE Common surgical treatments for trigeminal neuralgia (TN) include microvascular decompression (MVD), stereotactic radiosurgery (SRS), and radiofrequency ablation (RFA). Although the efficacy of each procedure has been described, few studies have directly compared these treatment modalities on pain control for TN. Using a large prospective longitudinal database, the authors aimed to 1) directly compare long-term pain control rates for first-time surgical treatments for idiopathic TN, and 2) identify predictors of pain control. METHODS The authors reviewed a prospectively collected database for all patients who underwent treatment for TN between 1997 and 2014 at the University of California, San Francisco. Standardized collection of data on preoperative clinical characteristics, surgical procedure, and postoperative outcomes was performed. Data analyses were limited to those patients who received a first-time procedure for treatment of idiopathic TN with > 1 year of follow-up. RESULTS Of 764 surgical procedures performed at the University of California, San Francisco, for TN (364 SRS, 316 MVD, and 84 RFA), 340 patients underwent first-time treatment for idiopathic TN (164 MVD, 168 SRS, and 8 RFA) and had > 1 year of follow-up. The analysis was restricted to patients who underwent MVD or SRS. Patients who received MVD were younger than those who underwent SRS (median age 63 vs 72 years, respectively; p < 0.001). The mean follow-up was 59 ± 35 months for MVD and 59 ± 45 months for SRS. Approximately 38% of patients who underwent MVD or SRS had > 5 years of follow-up (60 of 164 and 64 of 168 patients, respectively). Immediate or short-term (< 3 months) postoperative pain-free rates (Barrow Neurological Institute Pain Intensity score of I) were 96% for MVD and 75% for SRS. Percentages of patients with Barrow Neurological Institute Pain Intensity score of I at 1, 5, and 10 years after MVD were 83%, 61%, and 44%, and the corresponding percentages after SRS were 71%, 47%, and 27%, respectively. The median time to pain recurrence was 94 months (25th-75th quartiles: 57-131 months) for MVD and 53 months (25th-75th quartiles: 37-69 months) for SRS (p = 0.006). A subset of patients who had MVD also underwent partial sensory rhizotomy, usually in the setting of insignificant vascular compression. Compared with MVD alone, those who underwent MVD plus partial sensory rhizotomy had shorter pain-free intervals (median 45 months vs no median reached; p = 0.022). Multivariable regression demonstrated that shorter preoperative symptom duration (HR 1.005, 95% CI 1.001-1.008; p = 0.006) was associated with favorable outcome for MVD and that post-SRS sensory changes (HR 0.392, 95% CI 0.213-0.723; p = 0.003) were associated with favorable outcome for SRS. CONCLUSIONS In this longitudinal study, patients who received MVD had longer pain-free intervals compared with those who underwent SRS. For patients who received SRS, postoperative sensory change was predictive of favorable outcome. However, surgical decision making depends upon many factors. This information can help physicians counsel patients with idiopathic TN on treatment selection.
KEYWORDS:
BNI = Barrow Neurological Institute; Gamma Knife; IQR = interquartile range; MVD = microvascular decompression; RFA = radiofrequency ablation; Rhiz = partial sensory rhizotomy; SRS = stereotactic radiosurgery; TN = trigeminal neuralgia; UCSF = University of California, San Francisco; long-term outcome; microvascular decompression; pain; radiofrequency ablation; stereotactic radiosurgery; surgical outcome; trigeminal neuralgia
- PMID:
- 28298026
- DOI:
- 10.3171/2016.9.JNS16149


Dr. Newell,
Very very interesting. Please take a look at my digital magazine at http://www.infomeddnews.com
I am sure you remember me from the old Ekos Days. Kind regards, Pauline