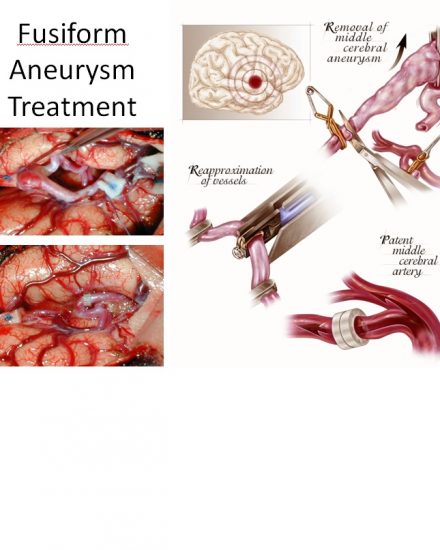
Brain Aneurysm | Cerebral Aneurysm. For help with symptoms, risks, and treatment options, contact our office.
Dr. David W Newell was born in Boston, MA and attended Case Western Reserve University Medical School. He completed his residency in neurosurgery at the University of Washington, including a year in London at St. George’s Medical School. Dr. Newell is the co-founder of the Swedish Neuroscience Institute and founder of the Seattle Neuroscience Institute.