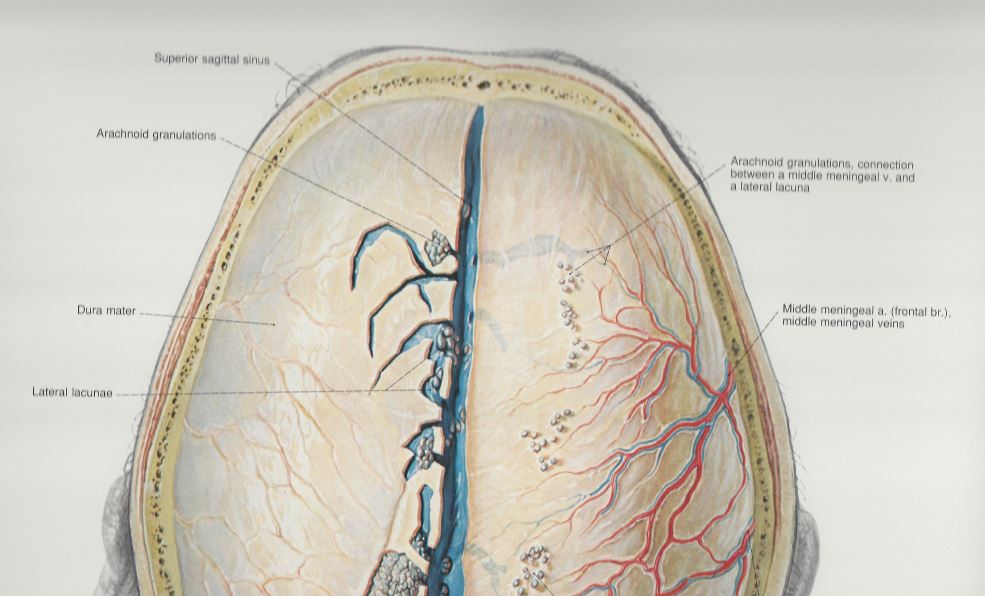
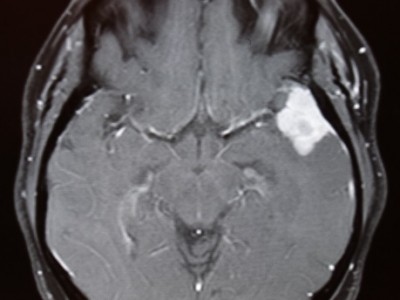
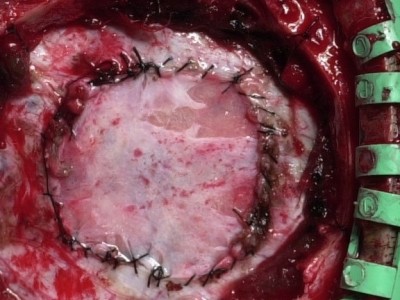
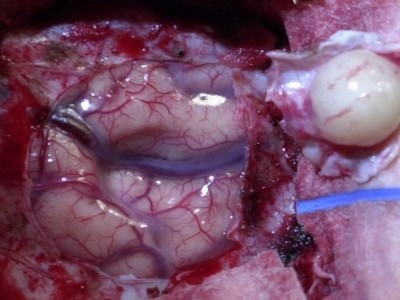
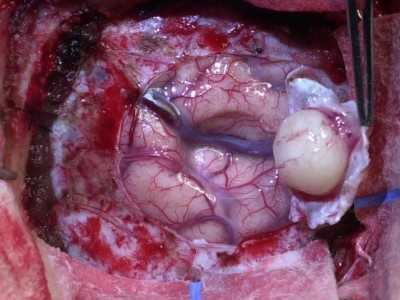
A meningioma is a tumor that grows from the dura which is part of the meninges. For help with symptoms, pain, risks, and treatment contact us or see Seattle Neurosciences’ website.
Dr. Newell was born in Boston, MA and attended Case Western Reserve University medical school. He then completed his residency in neurosurgery at the University of Washington, including one year in London at St. George’s medical school. Dr. Newell is the co-founder of the Swedish Neuroscience Institute and founder of the Seattle Neuroscience Institute.